SFMA is a comprehensive movement-based diagnostic system, moving beyond traditional methods, and identifying movement patterns linked to pain—a powerful tool for clinicians.
What is SFMA?
SFMA, or Selective Functional Movement Assessment, represents a groundbreaking shift in how healthcare professionals evaluate musculoskeletal issues. It’s not merely about identifying what hurts, but rather why it hurts, focusing on dysfunctional movement patterns. This system systematically filters out non-musculoskeletal sources of pain, like systemic inflammation, and pinpoints specific movement limitations contributing to a patient’s condition.
Unlike traditional assessments that often isolate individual structures, SFMA assesses the entire kinetic chain. It’s a clinical examination process designed to identify movement dysfunctions that may be the root cause of pain, even if the pain is felt elsewhere. The assessment utilizes a series of seven fundamental movements to reveal limitations and asymmetries.

The Need for Movement-Based Assessments
Traditional orthopedic and medical assessments frequently concentrate on identifying the specific tissues believed to be causing pain – a localized approach. However, this often overlooks the interconnectedness of the body and the role of movement dysfunction in pain generation. A movement-based assessment, like SFMA, acknowledges that pain is often a symptom of impaired movement, not necessarily structural damage.
This approach is crucial because it addresses the underlying cause of the problem, rather than just treating the symptoms. By identifying dysfunctional movement patterns, clinicians can develop targeted interventions to restore optimal movement and alleviate pain, leading to more effective and lasting results for patients.
SFMA vs. Traditional Assessments
SFMA distinguishes itself from traditional assessments by prioritizing movement patterns before focusing on specific tissues. Traditional methods often begin with palpation and special tests to pinpoint the source of pain, potentially missing broader movement impairments. SFMA, conversely, starts with a global movement screen to identify limitations and asymmetries.
This difference is significant because it shifts the focus from “what hurts” to “how does the patient move.” By identifying dysfunctional movements, SFMA guides clinicians toward the root cause of the problem, offering a more holistic and effective approach to diagnosis and treatment compared to solely addressing localized pain.
Core Principles of SFMA
SFMA centers on identifying movement dysfunction as the primary driver of pain, emphasizing regional interdependence and the crucial role of neuromuscular control.
Pain vs. Movement Dysfunction
SFMA fundamentally shifts the focus from pain as the problem, to pain being a symptom of underlying movement dysfunction. Traditional assessments often target painful areas directly, potentially missing the root cause. This approach acknowledges that pain can arise not from tissue damage alone, but from compromised movement patterns.
The assessment prioritizes identifying limitations in fundamental movements, even if pain isn’t immediately present during those movements. By uncovering these dysfunctions, clinicians can address the underlying mechanics contributing to pain, rather than solely treating the painful site. This distinction is crucial for effective, long-term patient outcomes, promoting functional improvements and reducing recurrence.
Regional Interdependence
SFMA recognizes the body as an interconnected system, emphasizing regional interdependence. This principle dictates that seemingly isolated impairments in one area can significantly impact movement and function elsewhere. A limitation in thoracic spine mobility, for example, might manifest as shoulder or hip pain due to compensatory strategies.
The assessment doesn’t treat body segments in isolation; instead, it evaluates how regional impairments influence global movement patterns. Clinicians must consider the entire kinetic chain when interpreting findings, acknowledging that dysfunction in one region can create stress and limitations in distant areas. This holistic perspective is vital for comprehensive treatment planning.
The Role of Neuromuscular Control
SFMA heavily emphasizes neuromuscular control as a cornerstone of functional movement. It’s not simply about identifying limited range of motion, but rather how movement is controlled and coordinated. Impaired neuromuscular control can lead to inefficient movement patterns, increased stress on joints, and ultimately, pain.
The assessment process aims to uncover underlying deficits in motor patterns, stability, and coordination. These deficits may stem from altered sensory input, impaired muscle activation, or inadequate motor planning. Restoring optimal neuromuscular control is crucial for long-term success, focusing on retraining the nervous system to facilitate efficient and pain-free movement.

The SFMA Examination Process
SFMA utilizes a systematic four-component examination, beginning with a global movement screen and progressing to selective and individualized assessments for diagnosis.
Overview of the Four Components
The SFMA examination is structured around four distinct, yet interconnected, components designed to systematically identify and address movement dysfunction. It begins with the Global Movement Screen, evaluating fundamental movement patterns like squats, lunges, and shoulder mobility. This initial screen helps pinpoint broad areas of limitation.
Next, the Selective Movement Assessment delves deeper, focusing on specific movements to isolate potential sources of pain and dysfunction within key regions. This is followed by the Individualized Movement Assessment, which refines the diagnosis by identifying painful arcs and provoking symptoms.
Finally, the Corrective Strategies component focuses on implementing targeted interventions, including self-correction techniques and manual therapy, to restore optimal movement and alleviate pain.
Component 1: Global Movement Screen
The Global Movement Screen serves as the initial filter in the SFMA process, assessing fundamental movement patterns to identify widespread limitations. It comprises four key tests: the Deep Squat, evaluating multi-segmental flexion; the Hurdle Step, assessing gait and coordination; the In-Line Lunge, examining single-leg stability and control; and Shoulder Mobility, checking overhead range of motion.
These movements are observed to identify compensatory strategies or asymmetries that may indicate underlying dysfunction. The goal isn’t to diagnose, but to highlight areas needing further, selective investigation. Positive findings trigger progression to Component 2.
Deep Squat
The Deep Squat is the first test within the Global Movement Screen, evaluating multi-segmental flexion of the hips, knees, and ankles. Clinicians observe for quality of movement, symmetry, and compensatory patterns. Common dysfunctions include limited ankle dorsiflexion, hip mobility restrictions, or trunk flexion limitations.
Assessing the deep squat reveals potential issues with core stability and neuromuscular control. A dysfunctional squat can indicate widespread movement impairments impacting functional activities. Observing depth, posture, and pain provocation guides further assessment within the SFMA framework.
Hurdle Step
The Hurdle Step assesses multi-planar hip and ankle mobility, along with coordination and balance during a functional stepping pattern. This test reveals limitations in hip flexion, ankle dorsiflexion, and single-leg stability. Observing step height, symmetry, and any compensatory movements is crucial.
Dysfunction during the hurdle step often indicates restrictions impacting gait and dynamic activities. Clinicians note if the patient struggles with control, exhibits excessive trunk lean, or demonstrates asymmetrical stepping. This observation directs the SFMA process towards specific regional assessments.
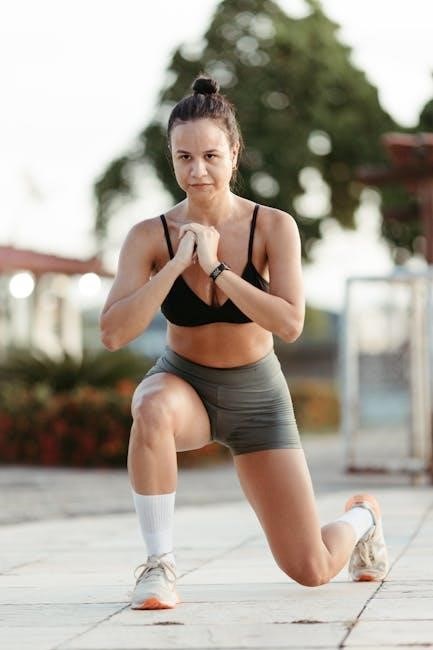
In-Line Lunge
The In-Line Lunge evaluates multi-segmental mobility and stability, specifically focusing on the lower extremity and core. It assesses anterior translation of the tibia, pelvic control, and overall balance during a weight-bearing, single-leg activity. Observing for valgus collapse, excessive trunk motion, or limited range of motion is key.
Limitations observed during this test can indicate restrictions in hip, knee, or ankle mobility, as well as core instability. The SFMA utilizes this assessment to pinpoint potential movement dysfunctions impacting functional tasks and guide further selective testing.
Shoulder Mobility
The Shoulder Mobility screen within the SFMA assesses bilateral shoulder flexion, evaluating range of motion and identifying potential asymmetries. This test reveals limitations in shoulder joint mechanics, thoracic spine mobility, or soft tissue restrictions impacting overhead movements.
Clinicians observe for compensations, such as scapular dyskinesis or trunk rotation, which suggest underlying movement impairments. Identifying restricted shoulder mobility is crucial, as it can contribute to pain and dysfunction in various activities. This assessment guides selective testing to determine the root cause of the limitation.
Component 2: Selective Movement Assessment
Component 2 of the SFMA delves deeper, utilizing selective movements to pinpoint the source of dysfunction revealed in the Global Movement Screen. This stage involves assessing specific movements – Cervical/Thoracic Rotation, Upper Extremity Flexion, Trunk Flexion, and Lumbar Flexion – individually.
The goal is to reproduce the patient’s pain during these controlled movements, identifying painful arcs and limitations. This component differentiates between regional and referred pain, guiding clinicians toward the primary driver of the patient’s symptoms. Careful observation and palpation are key during this focused assessment.
Cervical/Thoracic Rotation
Cervical/Thoracic Rotation within the SFMA’s Selective Movement Assessment specifically evaluates the range of motion and potential pain provocation during combined neck and upper back rotation; The clinician passively moves the patient through rotation, observing for asymmetries or painful arcs.
This assessment helps differentiate between local cervical issues and those originating from the thoracic spine, or even referred pain patterns. Identifying limitations or pain during this movement guides further investigation and potential treatment strategies focused on restoring optimal spinal mobility and reducing discomfort.

Upper Extremity Flexion
Upper Extremity Flexion, as part of the SFMA’s Selective Movement Assessment, assesses the shoulder’s ability to flex without compensation or pain. The clinician passively elevates the arm, observing for limitations in range of motion, scapular movement abnormalities, or the reproduction of symptoms.
This component helps pinpoint the source of upper extremity pain – whether it’s stemming from the shoulder joint itself, surrounding musculature, or referred from the cervical spine. Identifying painful arcs during flexion guides targeted interventions to restore proper shoulder mechanics and alleviate discomfort.
Trunk Flexion
Trunk Flexion within the SFMA’s Selective Movement Assessment evaluates the lumbar spine and surrounding tissues’ capacity for forward bending; The examiner passively flexes the patient’s trunk, carefully observing for asymmetries, restrictions, or pain provocation. This assessment aims to differentiate between true spinal limitations and compensatory movement patterns originating from other regions;
Identifying painful arcs during trunk flexion helps pinpoint the specific level of spinal involvement and guides targeted interventions. Clinicians analyze movement quality to determine if pain arises from muscular imbalances, joint restrictions, or underlying disc pathology, informing a tailored treatment plan.
Lumbar Flexion
Lumbar Flexion, a key component of the SFMA, specifically assesses the lower spine’s ability to bend forward. The clinician observes the patient’s movement, noting any limitations, asymmetries, or pain responses during passive flexion. This evaluation helps distinguish between genuine spinal restrictions and compensatory strategies employed by the patient.
Identifying painful arcs during lumbar flexion is crucial for pinpointing the source of discomfort. Palpation during the movement helps to identify specific tissues contributing to the pain, guiding targeted manual therapy or corrective exercises. The goal is to restore optimal lumbar movement and reduce pain.

Component 3: Individualized Movement Assessment
Component 3 of the SFMA dives deeper, moving beyond generalized screens to pinpoint specific pain generators; This phase focuses on identifying “painful arcs” – the specific ranges of motion where pain emerges during repeated movements. Clinicians systematically retest movements, carefully observing for patterns and limitations.
Provocation and Palpation are key here. Gentle pressure is applied to tissues during movement to determine if they reproduce the patient’s pain. This helps differentiate between joint, muscle, or ligament sources. The individualized assessment refines the diagnosis, guiding targeted treatment strategies.
Identifying Painful Arcs
Identifying Painful Arcs is central to the SFMA’s diagnostic process. Clinicians repeatedly perform movements, meticulously observing the range where pain first appears and its characteristics. This isn’t simply about where it hurts, but when during the motion pain is provoked.
These “arcs” provide crucial clues about the structures involved. For example, pain at the end-range suggests a ligamentous or capsular issue, while mid-range pain might indicate muscle or disc involvement. Precise identification guides subsequent provocation testing and treatment planning, ensuring specificity.
Provocation and Palpation
Following the identification of painful arcs, SFMA utilizes provocation and palpation to pinpoint the source of discomfort. Specific movements are repeated, but now with added stress or resistance, to confirm the suspected tissue involvement. This helps differentiate between referred pain and local pathology.
Simultaneously, careful palpation of relevant structures – muscles, tendons, ligaments, and joint capsules – is performed during these provocative maneuvers. The goal is to reproduce the patient’s pain with palpation, solidifying the diagnosis and guiding targeted interventions. This combined approach enhances diagnostic accuracy.
Component 4: Corrective Strategies
SFMA’s final component focuses on corrective strategies designed to address identified movement dysfunctions and alleviate pain. These strategies fall into two main categories: self-correction techniques and manual therapy interventions. Self-correction involves educating the patient on how to modify movement patterns, often using verbal cues and visual feedback.
Manual therapy, performed by the clinician, aims to restore proper joint mechanics and soft tissue mobility. This may include mobilization, manipulation, or myofascial release. The chosen approach is tailored to the individual’s findings, aiming to improve movement quality and reduce pain, ultimately restoring functional capacity.
Self-Correction Techniques
Self-correction techniques within the SFMA framework empower patients to actively participate in their recovery. These methods rely heavily on patient education, providing them with the understanding of how their movements contribute to their pain. Clinicians utilize verbal cues and analogies to guide patients toward optimal movement patterns, fostering body awareness.
Visual feedback, such as mirrors or video recordings, can further enhance self-correction. Exercises are often prescribed to reinforce these corrected movements, promoting long-term changes. The goal is to enable patients to independently manage their symptoms and prevent future recurrences through mindful movement.
Manual Therapy Interventions
Manual therapy interventions, guided by SFMA findings, address identified movement impairments. These techniques aren’t applied randomly; they’re specifically chosen to restore proper joint mechanics and tissue mobility. Common approaches include soft tissue mobilization to release restrictions, joint mobilization to improve range of motion, and muscle energy techniques to correct imbalances.
The focus isn’t solely on treating the painful area, but rather on addressing the underlying dysfunctional movement patterns. Manual therapy serves as a catalyst, facilitating the patient’s ability to implement self-correction techniques effectively, ultimately leading to lasting improvements.

SFMA Scoring and Interpretation
SFMA utilizes a standardized scoring system to quantify movement dysfunction, guiding clinicians in prioritizing treatment based on regional findings and pain patterns.
Understanding the Scoring System
The SFMA scoring system is designed to be objective and repeatable, providing a clear framework for assessing movement dysfunction. Each of the four components – Global Movement Screen, Selective Movement Assessment, Individualized Movement Assessment, and Corrective Strategies – contributes to the overall score. Scores aren’t about “passing” or “failing,” but rather identifying specific areas of limitation.
A score of 0 indicates no pain provocation during the movement, while higher scores (1-3) denote increasing levels of pain response. These scores pinpoint painful arcs of motion, guiding further investigation. The system emphasizes identifying the source of the dysfunction, not just the symptoms. Clinicians use these scores to track progress and adjust treatment plans effectively.
Interpreting Regional Findings
SFMA regional findings – cervical/thoracic, upper extremity, lumbar/pelvic, and lower extremity – offer crucial insights into movement impairments. Identifying the primary dysfunctional region is key; however, remember regional interdependence. Pain in one area doesn’t necessarily originate there. The assessment helps differentiate between local and referred pain sources.
For example, shoulder pain might stem from thoracic spine dysfunction. Interpreting findings requires considering the entire kinetic chain. A systematic approach, guided by the SFMA, allows clinicians to prioritize treatment based on the most significant movement limitations and pain provocation patterns, leading to targeted interventions.
Prioritizing Treatment Based on SFMA Results
SFMA results directly inform treatment prioritization, focusing on restoring optimal movement patterns. Address the most dysfunctional region first, as identified through the assessment process. Corrective strategies should target the painful arc and underlying movement impairments, not just the symptoms.
Begin with self-correction techniques, empowering patients to actively participate in their recovery. If self-correction is insufficient, manual therapy interventions can be employed. Re-assessment is crucial to monitor progress and adjust the treatment plan accordingly, ensuring a patient-centered and effective approach to rehabilitation.

Applications of SFMA
SFMA’s versatility extends to diverse fields, including sports and orthopedic rehabilitation, and pain management, offering targeted interventions for improved patient outcomes.
Sports Rehabilitation
SFMA proves invaluable in sports rehabilitation by pinpointing movement impairments directly contributing to athletic injuries. Unlike solely focusing on injured tissues, it assesses how the entire kinetic chain influences performance and risk of re-injury.
This approach allows therapists to develop individualized programs addressing fundamental movement deficiencies, not just symptoms. For example, a baseball pitcher with shoulder pain might exhibit limitations in thoracic spine rotation identified through SFMA. Correcting this foundational issue can improve mechanics and reduce stress on the shoulder.
By restoring optimal movement patterns, SFMA facilitates a faster, more complete return to sport, minimizing the likelihood of recurring problems and maximizing athletic potential.
Orthopedic Rehabilitation
In orthopedic rehabilitation, the SFMA offers a systematic approach to diagnosing and treating musculoskeletal conditions. It moves beyond traditional orthopedic assessments, which often isolate specific structures, to evaluate movement patterns as a whole.
This holistic view is crucial because pain and dysfunction rarely stem from a single source. SFMA helps identify regional interdependence – how limitations in one area impact others – guiding targeted interventions.
For instance, a patient with knee pain might have underlying hip or ankle mobility restrictions revealed by SFMA. Addressing these foundational issues can alleviate knee pain and improve overall function, leading to better long-term outcomes.
Pain Management
The SFMA proves invaluable in pain management by shifting the focus from solely treating symptoms to identifying the root causes of discomfort. It distinguishes between pain arising from genuine tissue damage and pain stemming from movement dysfunction.
By pinpointing dysfunctional movement patterns, clinicians can develop targeted corrective strategies, reducing pain and restoring optimal function. This approach is particularly beneficial for chronic pain conditions where traditional methods often fall short.
SFMA’s emphasis on movement allows for a more proactive and preventative approach to pain management, empowering patients to self-correct and maintain long-term relief.

Resources for SFMA Learning
SFMA certification courses, online materials, and recommended textbooks provide comprehensive training for healthcare professionals seeking to master this assessment tool.
SFMA Certification Courses
SFMA certification is achieved through rigorous, hands-on courses designed for healthcare professionals. These courses delve deeply into the assessment process, emphasizing practical application and clinical reasoning. Participants learn to accurately perform the four-component examination, interpret findings, and develop effective corrective strategies.
The curriculum focuses on identifying movement dysfunction as the root cause of pain, rather than solely addressing symptoms. Successful completion demonstrates proficiency in utilizing SFMA to guide treatment decisions and improve patient outcomes. Courses are frequently offered across the globe, providing accessible professional development opportunities. Certification ensures a standardized level of competence in this specialized assessment technique.
Online Resources and Articles
Numerous online platforms offer valuable resources related to the Selective Functional Movement Assessment. Websites dedicated to functional movement systems often host articles, videos, and case studies demonstrating SFMA application. Digital libraries and research databases provide access to peer-reviewed publications exploring the assessment’s validity and reliability.
Professionals can find supplementary materials, including downloadable guides and checklists, to enhance their understanding. Online forums and communities facilitate discussion and knowledge sharing among practitioners. These digital resources complement formal training, offering continuous learning opportunities and staying current with evolving best practices in movement assessment and rehabilitation.
Recommended Textbooks and Materials
For in-depth study of the Selective Functional Movement Assessment, several textbooks and materials are highly recommended. The official SFMA manual, published by Functional Movement Systems, provides a detailed overview of the assessment process, scoring, and interpretation. Complementary texts on functional anatomy, kinesiology, and neuromuscular control enhance understanding of underlying principles.
Consider resources focusing on movement impairments and corrective exercise strategies. Accessing case studies and clinical examples further solidifies practical application. While a direct “SFMA pdf” may be limited due to copyright, supplemental materials and research articles are widely available through professional organizations and academic databases.

